Biological hazards in food are the leading cause of foodborne illness worldwide. Every year, unsafe food sickens about 600 million people (almost 1 in 10 globally) and causes 420,000 deaths. These biological food hazards range from invisible pathogens to the toxins they produce, and they account for the vast majority of foodborne disease outbreaks.
The consequences aren’t just health-related; they’re also financial. Unsafe food costs an estimated $110 billion per year in productivity and medical expenses in low- and middle-income countries alone. In the United States, illnesses from major pathogens impose an annual burden of around $17.6 billion in healthcare, lost wages, and quality-of-life costs.
For food processors, these aren’t just public health tragedies; they’re also serious economic and brand risks, leading to costly recalls, lost consumer trust, and regulatory penalties. Whether you’re producing ready-to-eat (RTE) meals, dairy, meat, or fresh produce, or working in a QA or food safety role, understanding and managing biological food hazards is mission-critical.
In this guide, you’ll get ready-to-use hazard analysis templates, practical KPIs to measure biological hazard controls, and a step-by-step EMP plan aligned with FDA FSMA, everything you need to safeguard food safety compliance.
What are Biological Hazards in Food?
Biological hazards in food are living organisms or the substances they produce that can make humans sick when present in our food supply. In practical terms, this means pathogenic bacteria, viruses, parasites, and fungi (molds and yeasts) that contaminate food and cause illness. Unlike physical hazards (like metal fragments) or chemical hazards (like pesticides), biological food hazards are typically invisible to the naked eye. You can’t see, smell, or taste most microbial contaminants, which is why strict preventive measures are needed.
Biological Hazards vs. Contamination
It’s important to distinguish the hazard from contamination. A biological hazard is a pathogenic microorganism or its toxin that can cause harm. Contamination, on the other hand, is the event or condition by which that hazard enters the food. For instance, Listeria monocytogenes is a biological hazard; a dirty slicing machine that transfers Listeria into deli meat is the contamination route.
In essence, hazard is the danger, while contamination is the delivery mechanism. Your food can become contaminated at any point from farm to fork. Simply put: control the contamination, and you control the hazard.
Regulatory Compliance Context: Why Controlling Biological Hazards is a Legal Requirement
Controlling biological hazards isn’t only a food safety best practice; it’s a legal obligation. In the U.S. and globally, food processors, especially ready-to-eat (RTE) producers, must comply with laws that mandate preventive controls, validated processes, and rigorous monitoring. Two primary frameworks apply:
FDA Food Safety Modernization Act (FSMA)
FSMA requires preventive controls for human food, with a focus on hazard analysis and risk-based preventive measures. Signed into law in 2011, FSMA shifted U.S. food regulation from reactive to preventive. Under 21 CFR Part 117 (Current Good Manufacturing Practice, Hazard Analysis, and Risk-Based Preventive Controls for Human Food), processors must:
- Conduct hazard analyses, including biological hazards (Listeria, Salmonella, E. coli, etc.).
- Establish and monitor preventive controls (cooking, sanitation, allergen management).
- Implement Environmental Monitoring Programs (EMP) for RTE facilities.
- Maintain verification, validation, and recordkeeping systems.
Failure to comply can result in FDA warning letters, product recalls, facility suspension, or criminal liability.
HACCP Requirements for RTE Food
HACCP (Hazard Analysis and Critical Control Points) is a global standard that underpins FSMA. For high-risk foods (e.g., RTE, dairy, meat, produce), biological hazards are often classified as significant hazards requiring specific preventive controls.
For RTE foods, HACCP requires processors to:
- Identify biological hazards at each step.
- Define Critical Control Points (CCPs), such as cooking or chilling.
- Establish measurable critical limits.
- Monitor, verify, and document all CCPs.
Together, FSMA and HACCP form the backbone of U.S. compliance, ensuring processors actively prevent biological hazards rather than respond after contamination occurs.
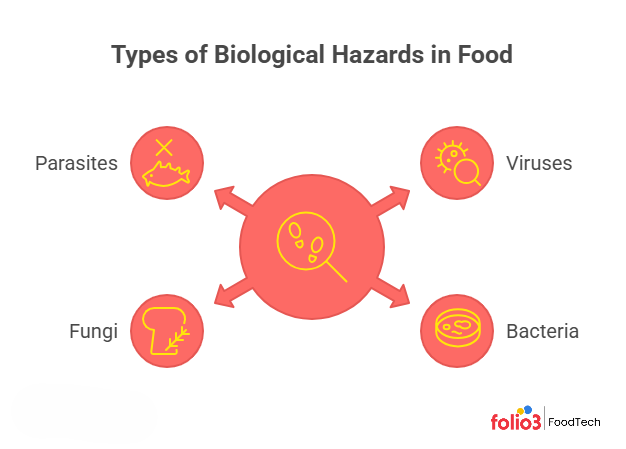
Types of Biological Hazards in Food
Biological hazards come in several forms. The four primary categories are viruses, bacteria, fungi, and parasites. Each type has distinct characteristics and sources, and understanding these differences will help you prevent food safety failures. Below, we break down each category with examples of common pathogens, the foods they affect, and why they’re a concern.
Viruses
Viruses are tiny infectious agents, much smaller than bacteria, that remain one of the most significant biological hazards in food. Unlike bacteria, they can’t multiply in food, but they survive long enough to infect you once consumed. In the U.S., norovirus alone causes about 58% of all foodborne illnesses, making it the leading cause of food poisoning. Norovirus and Hepatitis A are the two main culprits.
Unique Survival Traits
Viruses are remarkably resilient. They withstand acidic environments, freezing, and even heating up to 60 °C (140 °F). Noroviruses, in particular, can persist on surfaces for weeks and resist chlorine levels higher than those found in standard drinking water. These traits mean that quick steaming, light cooking, or acidic stomach conditions often do not destroy them.
Entry into the Food Chain
Viruses are typically of fecal origin and usually enter food through contaminated water, polluted shellfish beds, or infected food handlers. Irrigation or washing with unsafe water can deposit viruses like norovirus and Hepatitis A on fruits and vegetables. Shellfish such as oysters and clams concentrate viruses from polluted waters. Infected handlers who neglect proper hygiene can contaminate ready-to-eat foods like salads, sandwiches, or bakery items.
High-Risk Foods and Settings
Fresh produce, shellfish harvested from unsafe waters, and ready-to-eat foods handled after cooking are standard vehicles. Outbreaks in restaurants, cafeterias, and cruise ships illustrate how a single ill worker can spread billions of viral particles, with as few as 10–100 needed to cause infection.
Bacteria
Bacteria are single-celled microorganisms and among the most diverse biological hazards in food. Unlike viruses, many bacteria can multiply in food when conditions allow, which makes them a significant challenge in processing and storage. Pathogens of concern include Salmonella, E. coli O157:H7, Listeria monocytogenes, Campylobacter, Staphylococcus aureus, Bacillus cereus, Clostridium perfringens, and Vibrio parahaemolyticus. Illnesses can range from mild stomach upset to life-threatening infections.
Growth Conditions
Most bacteria thrive in moist, protein-rich foods and multiply quickly in the “danger zone” of 40 °F to 140 °F (4 °C to 60 °C). At ideal temperatures, some double every 20 minutes, which is why food safety rules emphasize keeping hot foods hot, cold foods cold, and limiting room-temperature exposure to no more than two hours.
Sensitivity to pH and Water Activity
Bacterial growth slows in acidic foods (below pH 4.6) and in products with low water activity. This is why pickles, jams, and dry foods like crackers or jerky rarely support bacterial hazards, though pathogens may survive in a dormant state and become dangerous once rehydrated or mishandled.
Spore Formation
Certain bacteria form spores that survive heat and drying. Bacillus cereus and Clostridium species can persist through cooking and later germinate, causing outbreaks in improperly stored cooked foods or in canned products without proper acidity or thermal treatment.
Common Bacterial Pathogens and Foods
- Salmonella: A leading biological food hazard in poultry, eggs, meat, and produce. Causes 1.35 million infections, 26,500 hospitalizations, and 420 deaths annually in the U.S.
- Campylobacter: Found in up to 50–70% of retail chicken. Causes gastroenteritis worldwide and spreads through undercooked poultry and cross-contamination.
- E. coli O157:H7 & STEC: Linked to undercooked beef, leafy greens, and raw milk. Can cause severe diarrhea and kidney failure, especially in children.
- Listeria monocytogenes: Grows at refrigeration temperatures. High fatality (≈20%) among pregnant women, newborns, the elderly, and immunocompromised individuals. Found in RTE meats, smoked fish, and soft cheeses.
- Staphylococcus aureus: Spread from human handling. Produces heat-stable toxins in foods like ham, pastries, and custards. Toxins survive reheating.
- Clostridium perfringens: Common in cooked meats, stews, or gravies that are cooled too slowly. Spores germinate and multiply, causing diarrhea and cramps.
- Bacillus cereus: Associated with rice or pasta left at room temperature. Causes vomiting (toxin in food) or diarrhea (toxin in the intestine).
- Vibrio species: Found in raw or undercooked seafood, especially oysters. V. vulnificus can be deadly to people with liver disease.
Fungi (Molds and Yeasts)
Fungi in food mainly include molds and yeasts. While yeasts usually cause spoilage, molds are a bigger biological food hazard because certain species produce dangerous mycotoxins. Both can grow in conditions where bacteria struggle, such as acidic or low-moisture foods.
Molds and Mycotoxins
Molds like Aspergillus, Fusarium, and Penicillium are visible as fuzzy growths, but the real threat lies in their toxins. Aspergillus flavus on peanuts or corn can produce aflatoxins, potent liver carcinogens. Fusarium on grains generates fumonisins and vomitoxin (DON). These toxins resist processing and can cause acute poisoning or chronic illnesses such as liver cancer and immune suppression. Globally, an estimated 25% of crops are contaminated with mycotoxins each year, with aflatoxin exposure contributing to high liver cancer rates in Africa and Asia.
Yeasts and Spoilage
Yeasts are single-celled fungi often responsible for off-flavors or unwanted fermentation in juices and pickles. Though rarely pathogenic, they spoil sugary or acidic foods.
Beneficial vs. Harmful Fungi
Not all fungi are hazards: yeasts ferment bread and wine, while molds help make cheese and tempeh. Problems arise when uncontrolled molds contaminate grains, nuts, spices, dried fruits, or RTE foods stored with excess moisture.
Parasites
Parasites are organisms that live on or in a host, drawing nourishment at the host’s expense. In food safety, the key concerns are parasitic worms (helminths) and protozoa transmitted through food or water. Though less common than bacteria or viruses, they can cause serious illness and remain a notable biological food hazard.
Trichinella spiralis: A roundworm once common in pork, now mainly in wild game. Causes trichinellosis with muscle pain and fever; can be fatal if untreated.
Tapeworms: Taenia solium (pork) and Taenia saginata (beef) spread via undercooked meat. Pork tapeworm eggs can cause cysticercosis, invading tissues and the brain. Diphyllobothrium tapeworms come from raw freshwater fish.
Protozoa: Microscopic parasites including Cryptosporidium, Cyclospora, Giardia, and Toxoplasma. Spread by contaminated water or produce.
- Cryptosporidium and Giardia are spread through water and or present in beverages; they cause diarrhea and can be severe in immunocompromised people.
- Cyclospora cayetanensis has caused numerous outbreaks via imported fresh produce like berries and salad mixes, causing protracted diarrheal illness.
- Toxoplasma gondii, which is often contracted from undercooked meat or soil contaminated by cats, is especially dangerous during pregnancy and is linked to about 20% of U.S. foodborne deaths.
Fish-borne Parasites: Raw or undercooked fish can carry parasites like Anisakis (a nematode worm) and Opisthorchiidae liver flukes. Certain Asian delicacies, like raw or undercooked freshwater fish, have led to liver fluke infections that can cause liver disease.
High-Risk Foods
Undercooked meats, raw seafood, wild game, and unwashed produce are standard vehicles. Imported produce from regions with poor food sanitation and safety mistakes, sushi made from improperly frozen fish, and leafy greens rinsed in unsafe water remain high-risk foods for parasite transmission.
How Biological Hazards Enter the Food Chain
Biological hazards can infiltrate foods at many points from farm to table. As a food safety planner, you should examine each link in your supply chain for potential contamination sources. Below are some major pathways through which pathogens and other biological agents enter the food chain:
Raw Materials
Ingredients and raw agricultural products often carry inherent microbial risks. Poultry frequently harbors Salmonella and Campylobacter, while crops may be contaminated by E. coli from wildlife feces or molds on grains. Raw milk often contains diverse bacteria. Without kill steps like cooking or pasteurization, raw materials become direct vectors. That’s why HACCP plans emphasize supplier controls and specifications, such as requiring pathogen testing on nuts or verifying GAPs for produce.
Water Systems
Water touches nearly every process, washing, cooling, or serving as an ingredient. Contaminated irrigation water can deposit Cyclospora or Salmonella on produce, while process water in flumes or ice machines can spread microbes if sanitizer levels drop. Backflows or wet drains may introduce Listeria into equipment. Safe water supply, antimicrobial treatments, and routine testing are essential to controlling this hazard.
Food Handlers
People remain one of the most significant contamination sources. Ill or unclean employees may spread norovirus, Hepatitis A, or Staphylococcus aureus through poor hygiene. Simple lapses touching the nose before handling deli meat can contaminate ready-to-eat foods. Strict handwashing, illness reporting, glove use, and training are vital safeguards.
Equipment & Surfaces (Biofilms)
Unclean or poorly designed equipment can harbor biofilms that shed bacteria into food. Examples include Listeria in slicers or Salmonella in cutting machines. Sanitary equipment design, thorough cleaning, and environmental swabbing are critical.
Air and HVAC Systems
Airborne hazards can affect dry products like powdered milk or spices, spreading Salmonella or Cronobacter. High-pressure washing may aerosolize Listeria from drains. Mold spores also travel via poorly maintained HVAC. Controls include HEPA filtration, positive air pressure, and separate air handling for raw vs. RTE zones.
Cross-Contamination
Cross-contact happens when pathogens transfer between raw and finished products, such as when chicken drips on salad or when utensils are reused without cleaning. Poor zoning and traffic patterns in plants exacerbate risks. Preventive measures include color-coded equipment, sanitation between uses, and strict zoning.
Post-Process Contamination
Even after cooking or pasteurization, hazards can re-enter during cooling or packaging. Contaminated fillers, gloves, or packaging rooms have introduced Listeria and Salmonella into finished goods. High-hygiene zones, UV tunnels, container sealing, and daily monitoring help prevent these late-stage hazards.
Preventive Strategies for Biological Hazard Food Safety
How to prevent biological hazards in food? Knowing the enemy (the hazards and entry points) is half the battle. The other half is implementing effective preventive strategies to control and eliminate those biological hazards in food production. A robust food safety system is built on multiple layers of defense. Here we outline key control measures in a structured way:
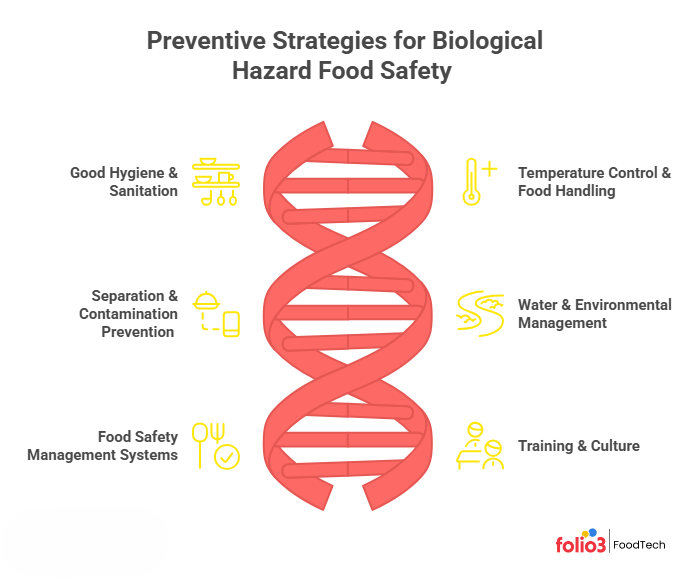
1. Good Hygiene & Sanitation
Maintaining strict hygiene and sanitation is the foundation of biological hazard food safety. Think of it as creating a hostile environment for pathogens so they have minimal opportunity to survive or spread.
Personal Hygiene: Mandatory handwashing at critical points, clean uniforms, and hair/beard nets are essential. Proper 20-second handwashing prevents nearly a third of diarrheal illnesses [CDC]. Gloves help but require strict discipline.
Illness Policies: Exclude workers with vomiting, diarrhea, jaundice, or fever. A 24–48-hour symptom-free period before returning minimizes virus or bacteria shedding.
Facility Hygiene Design: Provide handwash stations with soap and hot water. Use foot pedals or sensors to avoid recontamination and sanitizing barriers at zone transitions.
SSOPs: Follow strict cleaning schedules between shifts. Use detergents to remove soil and apply approved sanitizers like chlorine, quats, or peracetic acid. Verify with ATP or microbial swabs.
Sanitary Facility Design: Ensure non-porous surfaces, sloped drains, and sealed cracks. Equipment should be off the walls and free of harborages.
Microbial Monitoring: Routine swabs, especially in RTE zones, help detect Listeria or indicators early, triggering corrective action before hazards spread.
2. Temperature Control & Food Handling
Since most bacteria and some other pathogens are susceptible to temperature, controlling temperature is one of the most powerful safety measures in our arsenal. It includes both cooking (lethality steps) and holding (prevention of growth).
Cooking/Processing to Destroy Hazards: Validate kill steps such as cooking, pasteurization, or high-pressure processing. For instance, milk pasteurization at 72 °C for 15 seconds eliminates resistant pathogens. Low-moisture foods require stricter parameters. Keep batch records of time, temperature, and pressure.
Chilling and Refrigeration: Rapid cooling prevents growth of spore-formers like C. perfringens. Follow standards: 135 °F to 70 °F within 2 hours, and to 40 °F within 6 hours. Cold-chain foods must remain at ≤40 °F.
Hot Holding: Maintain ≥140 °F during hot holding until packaging or service. Use steam tables, warmers, or insulated systems to keep food safe.
Avoiding Temperature Abuse: Minimize time in the danger zone (40–140 °F). Avoid leaving raw or cooked food at room temperature. Plan efficient workflows from cooler → process → cooler.
Freezing for Parasite Control: Use freezing to kill parasites in raw seafood, meeting regulatory requirements for sushi-grade fish.
Thermometer Use and Calibration: Provide calibrated thermometers and train staff in correct use. Regularly verify accuracy using ice water or boiling tests.
Temperature Monitoring Systems: Employ continuous monitoring in storage and transport with data loggers or IoT sensors to protect the cold chain.
3. Separation & Cross‑Contamination Prevention
The mantra is “Keep raw and RTE separate – in space or in time (with cleaning)”. By doing so, you significantly reduce the chances that a pathogen present in raw ingredients will hitchhike into your finished product, which may not have another kill step.
Facility Zoning: Keep raw and RTE products in distinct zones or schedule production with complete cleaning between. Use floor markings or signage to delineate areas.
Equipment Separation: Dedicate tools to specific tasks, using color-coding (e.g., red for raw meat, green for vegetables). If sharing is unavoidable, sanitize thoroughly between uses.
Personnel Practices: Control movement between zones. Require smock changes, footbaths, or strict handwashing. Some plants enforce one-way flows from raw to RTE areas.
Utensil and Surface Sanitation: Define strict cleaning before surfaces or utensils switch from raw to cooked use. Time separation (e.g., raw at day’s end) adds protection.
Physical Barriers: Use curtains, partitions, or separate counters to prevent direct cross-contact.
Workflow and Utensil Control: Keep raw containers and tools away from finished products—color-code cleaning tools to prevent cross-use.
Airflow and Pressure: Maintain positive pressure in RTE areas to prevent airborne contamination.
Cross-Contact in Processing Aids: Never reuse marinades or utensils from raw products on cooked foods without a kill step.
4. Water & Environmental Management
Beyond direct product contact issues, controlling the broader food processing environment, particularly water, waste, and surroundings, is essential for preventing biological hazards. By treating the environment and utilities with the same care as direct food contact, you close off many “back door” routes that hazards use to infiltrate.
Water Quality Management: Test wells routinely and treat with chlorination or UV if needed. Recirculated water must be disinfected, monitored for pH and sanitizer levels, and systems cleaned regularly to prevent biofilms.
Drains and Sewage Control: Design drains to flow away from product zones. Clean and sanitize frequently, use foaming agents, and avoid spraying hoses directly into drains to prevent aerosols.
Avoiding Standing Water: Fix leaks promptly. Remove puddles and favor dry cleaning in low-moisture areas. If wet cleaning is necessary, follow with thorough drying.
Waste Management and Traffic: Remove waste quickly in covered bins. Keep traffic patterns so waste never passes through clean zones. Use sanitizing mats or barriers at entries.
Pest Control: Pest control can seal building gaps, employ traps, and maintain sanitation to deny pests food or water.
Preventing Entry of Environmental Pathogens: Filter incoming air, keep doors closed, and enforce hygiene for maintenance staff.
Surroundings: Maintain outdoor areas: trim grass, remove standing water, and position dumpsters away from entrances.
5. Food Safety Management Systems
Beyond individual practices, you need an overarching Food Safety Management System (FSMS) to organize and verify all these controls. In essence, an FSMS like HACCP/HARPC ties together all the specific good practices into a coherent, monitored program.
HACCP Plan: Implement a HACCP or preventive control plan to identify hazards, set critical limits, and monitor controls. For example, in canning, C. botulinum is controlled by validated retort times and temperatures.
Validation and Verification: Validate measures with scientific data or guidance. Verify CCPs through calibration checks, log reviews, or microbial tests—audit prerequisite programs with swabs or pest reports.
Documentation and Record-Keeping: Maintain thorough records of cooking temps, sanitation schedules, and training. Digital systems simplify trending and food safety audits.
Internal Audits: Regular self-audits catch gaps before regulators or outbreaks do.
Continuous Improvement: Use data, complaints, or swab results to identify root causes and tighten controls over time.
6. Training & Culture
Even the best-designed controls can fail if humans don’t execute them properly. That’s why training and fostering a food safety culture are perhaps the most pivotal elements.
Initial and Ongoing Training: Provide role-specific training on hygiene, sanitation, cooking/cooling, and allergen control. Use a mix of hands-on demos, posters, and refreshers annually or when procedures change.
Empowerment to Speak Up: Encourage staff to report hazards without fear. A culture where stopping the line for safety is praised ensures accountability.
Lead by Example: Supervisors must model compliance, washing hands, wearing PPE, and coaching during Gemba walks. Leadership behavior sets the tone.
Culture Building: Embed food safety into KPIs, celebrate milestones, and share outbreak stories to stress real-world consequences.
Simplify and Provide Resources: Stock supplies, post clear signage, and streamline tasks. Easy systems boost compliance.
Team Involvement: Engage employees in solving issues, like persistent swab failures, to build ownership.
External Training and Certification: Support HACCP, PCQI, or conference participation to grow expertise.
Sector‑Specific Control Measures to Avoid Biological Food Hazards
What are examples of biological hazards in food? Different sectors of the food industry face unique biological hazards based on their products and processes. While the general principles of food safety apply everywhere, there are some customized strategies and focal points for various categories of foods. Let’s look at a few:
Ready‑to‑Eat (RTE) Foods
Examples: Deli meats, salads, smoked fish, sandwiches, prepared meals – foods that are eaten without further cooking by the consumer.
Primary Hazards
Listeria monocytogenes is the most critical hazard in RTE foods because it survives refrigeration, and there’s no kill step before consumption. Other risks include Staphylococcus aureus (if growth is allowed post-handling), Clostridium botulinum (in anaerobic packaging under abuse), and post-process contamination by Salmonella or E. coli. Viruses like Hepatitis A and Norovirus may enter via infected handlers.
Controls
RTE operations must enforce strict zoning to keep raw ingredients separate from post-kill areas. Routine Listeria swabbing of Zone 2 & 3 surfaces is essential, with corrective actions if positives appear (deep cleaning, intensified swabbing, Zone 1 checks). USDA requires either post-lethality treatments or robust sanitation plus testing.
Dairy Processing
Examples: Milk, cheese, yogurt, ice cream, powdered milk.
Primary Hazards
Raw milk may carry Salmonella, E. coli, Listeria, Campylobacter, and more. Pasteurization is critical, but post-process risks remain: Listeria in soft cheeses, Salmonella or Cronobacter in powders, and toxins from Staph aureus or C. botulinum in improperly handled dairy.
Controls
Pasteurization is the cornerstone of dairy safety, legally required in many countries. Post-pasteurization, thorough cleaning, and validated CIP systems prevent recontamination. Dry plants use environmental swabbing to detect Cronobacter or Salmonella without adding moisture. Strict zoning, filtered positive-pressure air, footbaths, and separate tools reinforce hygiene. Rapid cooling and specific starter cultures in fermented products further suppress pathogens.
Meat & Poultry
Examples: Slaughterhouses, ground meat processing, poultry cutting, further processed meats (sausages, ham).
Primary Hazards
Raw meat and poultry naturally harbor Salmonella, Campylobacter, and E. coli O157. Risks include Clostridium perfringens or C. botulinum in processed meats if abused, Staphylococcus aureus from temperature abuse, and Listeria post-cook in RTE meats. Improper cooling can also enable Bacillus cereus or C. perfringens growth.
Controls
At slaughter, inspection and contamination control are critical. Beef plants use hide removal hygiene, organic acid rinses, steam vacuums, and hot water pasteurization to reduce pathogens. Poultry relies on chiller chlorination and cold temperatures under USDA Salmonella performance standards. In processing, maintain strict hygiene: clean equipment, limit room-temp exposure, treat trim before grinding, and schedule higher-risk products last to allow thorough cleaning.
Bakery & Grain Products
Examples: Breads, cakes, dry cereals, flour, baking mixes, pasta.
Primary Hazards
Baking kills most pathogens, but raw flour is a key risk, linked to E. coli and Salmonella outbreaks in cookie dough and mixes. Post-baking contamination is another concern, while finished dry products resist bacterial growth but may spoil if moisture allows mold.
Controls
Baking is the key step, validated for dense products to ensure even heating. Spores rarely germinate in dry goods, but mishandling (warm, moist bread) poses a risk. For raw flour mixes, use heat-treated flour; nuts should be pasteurized. Pasteurized eggs are essential in uncooked icings. In dry facilities, control Salmonella with environmental monitoring and dry-cleaning methods, thoroughly drying if water is used.
Produce & Fresh‑Cut
Examples: Fresh fruits, vegetables, salads, cut fruits, ready-to-eat packaged produce.
Primary Hazards
Raw produce can carry E. coli O157:H7, Salmonella, Listeria, Shigella, Cyclospora, Cryptosporidium, Hepatitis A, and Norovirus from contaminated fields or water. With no kill step, contamination persists—seen in outbreaks from romaine, melons, cantaloupe, salad mixes, and frozen berries.
Controls
Prevention begins with Good Agricultural Practices (GAPs): safe irrigation water, livestock exclusion, proper manure composting, and worker hygiene. Many processors mandate GAP audits. At packing, sanitize wash water (chlorine, peracetic acid, ozone) and monitor levels closely. Use counter-flow rinses to avoid cross-contamination. Rapid precooling (hydro or vacuum cooling) and strict cold storage slow pathogen growth and preserve produce quality.
Detection & Testing Methods to Avoid Biological Hazards in Food Processing
Preventive measures are essential, but “trust and verify” is the innovative approach. Detection and testing methods help verify that your controls are working and alert you to potential hazards before products reach consumers. It includes both environmental and product testing, as well as rapid detection technologies and data analysis for trends.
Environmental Monitoring Program (EMP)
An EMP systematically tests production environments (surfaces, drains, air, water) to catch pathogens before they reach food. RTE plants often swab for Listeria spp. in drains and floors or Salmonella in dry areas.
Risk-based sampling sites: Focus on drains, niches, and residue-prone areas; rotate and randomize swabs.
Pathogen vs. indicator testing: Many tests for Listeria spp. as an indicator, escalating to L. monocytogenes confirmation if on food contact surfaces.
Frequency: Zone 1 surfaces may be periodic; Zones 2/3 are tested daily or weekly.
Responsive actions: Positives trigger immediate deep cleaning, retesting, and root cause checks.
Record-keeping and mapping: Track swabs, results, and trends; use maps/heat charts to spot hotspots.
Product & Ingredient Testing
Testing the food products or ingredients themselves for pathogens or spoilage organisms is another layer of protection. It’s especially crucial for high-risk items or items that won’t undergo a kill step later.
Ingredient testing: Require Certificates of Analysis (COAs) for high-risk inputs (e.g., Salmonella in spices, Cronobacter in dairy powders). Some plants quarantine lots until in-house tests clear them.
In-process testing: Use checks like silo milk coliform counts or fermentation pH to confirm processes are working.
Finished product testing: Often applied to RTE items as “test and hold” for Listeria in deli meats, mandatory Cronobacter tests in infant formula.
Indicator organisms: Coliforms, APC, or Enterobacteriaceae signal hygiene lapses.
Shelf-life/challenge studies: Validate formulations by storing under abuse conditions or spiking with pathogens.
Rapid tests: ATP swabs, immunoassays, and PCR enable faster verification and “hold-and-release” programs.
Rapid Methods & Verification Tools
Technology has improved detection speed and convenience, which is crucial because holding a product for days waiting for results is costly.
Rapid pathogen detection: Traditional culture takes 3–5 days; rapid PCR or immunoassays give results in 24–48 hours, cutting warehouse time. AOAC-approved PCR kits and emerging biosensors are widely used.
Whole genome sequencing (WGS): WGS links isolates to outbreaks with genetic precision. Companies use it to distinguish recurring resident strains from new introductions.
Automation and continuous monitoring: IoT and automated sensors log CCPs like pasteurization or chilling, flagging deviations instantly.
Sanitation verification: ATP swabs or protein tests verify cleaning in minutes; failures trigger immediate recleaning.
Online analyzers: Inline detectors (UV for aflatoxin, coliform monitors) ensure on-the-fly quality.
Data management and analysis: Analytics trend, swab and test results, highlighting hotspots or recurring issues.
How Folio3 FoodTech Automates Detection & Prevention with Food Safety Software
Modern food safety is bolstered by technology and software that help manage the complexity of hazard controls. Managing biological hazards like Salmonella, Listeria, and E. coli is one of the toughest challenges for food processors. Manual logs, fragmented systems, and reactive approaches leave gaps that pathogens can exploit.
A food safety software by Folio3 Foodtech transforms this process by giving you automation, real-time insights, and complete control across your operations. Here’s how our solutions can help operationalize and automate the detection and prevention of biological hazards:
Environmental Monitoring & Sanitation Verification: Stay ahead of risks using digital EMPs, heatmaps, and instant alerts, so contamination is contained before it threatens your products.
Mobile Compliance Management & Digital Checklists: Replace paper logs with mobile checklists that flag issues instantly, ensuring your team never misses a critical food safety step.
Quality Management & CAPA Tracking: Turn every positive test into action with automated corrective workflows that assign tasks, track resolution, and prevent recurrence permanently.
Traceability & Recall Management: Trace every ingredient and batch within minutes, enabling rapid recalls and transparent reporting to protect both your brand and consumers.
IoT and Sensor Integration: Real-time temperature, humidity, and process sensors notify you instantly when conditions drift, preventing pathogen growth before it compromises safety.
AI & Predictive Analytics: Leverage AI to spot contamination patterns and seasonal trends, empowering you to prevent hazards before they escalate into costly recalls.
Ready to elevate your food safety program? Contact Folio3 FoodTech today for a demo of how our end-to-end food safety and quality platform can be tailored to your operation and take your biological hazard prevention to the next level with automation, intelligence, and ease-of-use.
Frequently Asked Questions on Biological Hazards in Food Safety
Which Task May Cause Biological Hazards that Can Contaminate Food?
Any task that brings pathogens into contact with food can introduce biological hazards. Examples include handling raw meat or poultry near RTE products, using contaminated water for washing produce, poor employee hygiene, or inadequate cleaning of slicers, mixers, or drains. Even something as simple as a worker skipping handwashing after a restroom break can spread norovirus or Salmonella to ready-to-eat foods.
Which Biological Hazards are Most Common in RTE Manufacturing?
The top concern for RTE facilities is Listeria monocytogenes, as it thrives in cold, wet environments and grows in refrigeration. Other common hazards include Salmonella, E. coli O157:H7, and Staphylococcus aureus if hygiene breaks down. Viruses like Hepatitis A or Norovirus from ill food handlers also pose significant risks.
How often Should We Swab in Zones 1–4?
Zone 1 (direct food contact surfaces) should be swabbed regularly, often daily or weekly, depending on risk. Zones 2–4 (adjacent equipment, floors, drains, walls) can be swabbed on a rotating schedule, but at least weekly for Zone 2 and monthly for lower-risk areas. Frequency should always be risk-based and validated through trend analysis.
Is ATP Enough to Prove Sanitation for Pathogen Control?
No. ATP swabs are great for verifying cleanliness, but don’t confirm pathogen elimination. They detect organic residues, not specific bacteria like Listeria or Salmonella. An ATP “pass” should be combined with microbiological swabbing as part of your Environmental Monitoring Program (EMP) to truly confirm sanitation effectiveness.
When Should We Revalidate Our Kill Step or Cleaning Procedure?
Revalidation is essential whenever there’s a significant change, such as new equipment, altered recipes, modified cleaning chemicals, or adjusted time/temperature parameters. Even without changes, best practice is to revalidate kill steps (like pasteurization) and cleaning protocols at least annually, or sooner if trends in testing suggest risk.







